Healthcare Transparency As A Blockbuster Drug
Posted: February 2, 2015 Filed under: Just Culture, Leadership, Patient Safety, Transparency | Tags: Healthcare, Leadership, Lucian Leape Institute, Transparency Leave a comment“If transparency were a medication, it would be a blockbuster, with billions of dollars in sales and accolades the world over. While it is crucial to be mindful of the obstacles to transparency and the tensions—and the fact that many stakeholders benefit from our current largely nontransparent system—our review convinces us that a health care system that embraces transparency across the four domains will be one that produces safer care, better outcomes, and more trust among all of the involved parties. Notwithstanding the potential rewards, making this happen will depend on powerful, courageous leadership and an underlying culture of safety.”
 The previous paragraph comes from the fifth and final National Patient Safety Foundation’s Lucian Leape Institute (LLI) White Paper entitled, “Shining a Light: Safer Health Care through Transparency”. Each of the five white papers address key issues that healthcare stakeholders will need to successfully manage if healthcare is to achieve zero preventable harm. I was honored to be part of the panel that helped create this paper and the 39 recommendations for greater transparency throughout healthcare.
The previous paragraph comes from the fifth and final National Patient Safety Foundation’s Lucian Leape Institute (LLI) White Paper entitled, “Shining a Light: Safer Health Care through Transparency”. Each of the five white papers address key issues that healthcare stakeholders will need to successfully manage if healthcare is to achieve zero preventable harm. I was honored to be part of the panel that helped create this paper and the 39 recommendations for greater transparency throughout healthcare.
Defining transparency as “the free, uninhibited flow of information that is open to the scrutiny of others”, the paper provides recommendations in four different domains of transparency:
- Transparency between clinicians and patients (illustrated by disclosure after medical errors)
- Transparency among clinicians themselves (illustrated by peer review and other mechanisms to share information within health care delivery organizations)
- Transparency of health care organizations with one another (illustrated by regional or national collaboratives)
- Transparency of both clinicians and organizations with the public (illustrated by public reporting of quality and safety data)
I encourage everyone to visit the LLI website and download the White Paper (click here for a copy). Increased transparency is critical to any Patient Safety mission. Greater transparency throughout the system is not only ethically correct, but will lead to improved outcomes, fewer errors, more satisfied patients, and lower costs.
What Does Transparency in Healthcare Mean to You?
Posted: July 30, 2014 Filed under: Just Culture, Leadership, Medical Education, Transparency | Tags: Leadership, Medical Education, Mindfulness, Nursing education, Telluride Patient Safety Summer Camp, Transparency 1 CommentYesterday’s afternoon discussion at Telluride East was focused on “Transparency”, a buzzword for many in healthcare today, but a concept that holds tremendous meaning for patient safety and caregiver well-being for those who walk the talk. Dave Mayer started the conversation by asking the group to share what transparency meant to them, and then breaking up the larger group to discuss:
- What are the barriers to transparency in healthcare?
- What are the barriers to being transparent with patients?
- What are the benefits to having a transparent culture in place?
In our small group, several themes emerged, and surprisingly, not the least of which revolved around leadership and culture being the primary drivers of the “shades of transparency” experienced by both providers and patients in any given health system. One of our student scholars shared how he feels his excellent intuition, or spidey senses, need to be kept in check so as not to appear a “pain in the butt” to senior physicians–physicians who set grades and can directly impact his medical career. Those same spidey senses activated in the mindful physician during the delivery of care, or as he coined it, hypervigilence, are exactly what is being called for in healthcare organizations seeking to become high reliability systems. Here was someone who clearly was acting in the best interest of a patient, and because of hierarchy and poor leadership, was made to feel as though his intuition was a bad thing.
In a related and revealing post, I’m sick and tired…but far from done, Telluride faculty and colleague, Richard Corder, shares his ire related to watching the bad eggs of healthcare remain in place, to continue to harass and cripple the well-meaning efforts at culture change. While he comes from a position of understanding “the why” of the situation, he’s also sick and tired, as are many well-intentioned caregivers who have chosen to remain silent in the face of leadership that fails to lead–and worse yet–infuses toxicity into a culture and careers of those less tenured. When I hear stories like these I know we still have a long way to go to create a healthcare that is safe for all who work within it, or enter it as a patient.
The silver lining to all this is the medical and nursing students who have chosen to come to Telluride this year. The same medical student mentioned above also stated, “when I’m an attending, I will encourage questions about the care being delivered.” And I believe him, but I also know the real world sometimes takes that passion, that resolve, and turns it into “shades of the self” that if not careful, can turn even the most well-meaning individual into someone who has to rationalize or tone down the goodness within. It’s our job as healthcare leaders to support those young learners in any possible way we can. This is a recurring theme that comes to light at the Telluride Patient Safety Summer Camps…
Communication at Center of #TPSER10 Day One Discussions
Posted: June 10, 2014 Filed under: Education Technology, Healthcare Innovation, Patient Advocacy, Patient Centered Care, Patient Safety, Storytelling, Transparency | Tags: open honest communication, Patient Safety, Telluride Patient Safety Resident Summer Camp, Transparency 1 Comment Each year in Telluride, we kick off the week’s conversation on open and honest communication in medicine by showing the Lewis Blackman Story. For the 10th year in a row, Helen Haskell, Lewis’ mom, was part of the Telluride faculty and for the third year, led the post-film discussion along with Telluride Patient Safety Student and Resident Summer Camp founder, Dave Mayer MD. Many of the resident scholars commented on the various levels of communication failure that occurred during Lewis’ care. Doctor to patient communication, provider to provider communication, power gradient communication challenges–it has been clear for some time that being uncomfortable communicating with anyone in the circle of care to patients puts the patient, and also caregivers, at risk. Lewis’ case is an unfortunate example of what goes terribly wrong when open, honest communication is not valued in a health system.
Each year in Telluride, we kick off the week’s conversation on open and honest communication in medicine by showing the Lewis Blackman Story. For the 10th year in a row, Helen Haskell, Lewis’ mom, was part of the Telluride faculty and for the third year, led the post-film discussion along with Telluride Patient Safety Student and Resident Summer Camp founder, Dave Mayer MD. Many of the resident scholars commented on the various levels of communication failure that occurred during Lewis’ care. Doctor to patient communication, provider to provider communication, power gradient communication challenges–it has been clear for some time that being uncomfortable communicating with anyone in the circle of care to patients puts the patient, and also caregivers, at risk. Lewis’ case is an unfortunate example of what goes terribly wrong when open, honest communication is not valued in a health system.
For those of you who haven’t heard Lewis’ story–he is someone you would have loved to have met. He would be 28 years old this year had his path not crossed that surgical suite almost 14 years ago. An actor, a scholar, an athlete — a lover and friend of the underdog–Lewis was the teen you hoped your kid was hanging out with when you weren’t around. By all accounts, Lewis’ was poised to do wonderful things and he left his mark on life early through his caring, thoughtful nature, a witty sense of humor, a loving son and brother, and now an inspiration to many of us trying to make care safer for patients today. He is one of many who serve as an example of continued and senseless loss in our slow movement toward zero preventable harm in healthcare. We need to decide today, that it’s time to take action in new ways to prevent the same stories from repeating.
For example, what can we do to improve our professional communication skills among healthcare teams so that we ensure families like Lewis’ do not suffer a similar loss? So that good, conscientious caregivers are not put through the traumatic experience of harming a patient out of fear of speaking up in a toxic culture? Which medical education programs are stepping up to incorporate interpersonal communication skill building into their core curriculum from the first day of medical school? Please share best practices in teaching medical and nursing student communication, and start an open conversation about better ways to teach communication to care providers at every level.
A Video Learning Library for Quality & Safety in Healthcare via MedStar Health
Posted: February 27, 2014 Filed under: Healthcare Innovation, Leadership, Medical Education, Patient Safety, Storytelling | Tags: Dave Mayer MD, Healthcare innovation, High Reliability Organizations, Larry Smith, Learning Culture, MedStar Health, Poudre Valley Hospital, Transparency, William Neff MD, YouTube Leave a commentEach quarter, in the spirit of a learning culture inherent to high reliability organizations, MedStar Health Quality, Safety & Risk Management leadership, Dave Mayer MD and Larry Smith, host a retreat for quality and safety professionals, inviting outside speakers to share their expertise and discuss topics related to patient safety, risk management and improving healthcare quality. Those topics have included:
- Care for the Caregiver
- Human Factors Engineering
- High Reliability Organizations
- Patient & Family Stories
- Open, Honest Communication & Transparency
- Patient Engagement
- Baldrige Journey
MedStar Health has created a Video Learning Library on their website which includes a full recording of many of these sessions. The intention is to share the knowledge with all healthcare colleagues so that others can also benefit from the experience shared by these safety and quality thought leaders. The Library can be found on the MedStar Health website. Following is an example of the content, as Dr. Bill Neff, CEO & CMO, University of Colorado Health, shares the Baldrige Journey as experienced by Poudre Valley Hospital. Please share this resource with others!
Continuing a Journey That Seeks High Reliability
Posted: February 24, 2014 Filed under: High Reliability Organizations, Just Culture, Leadership, Uncategorized | Tags: Cincinnati Children's Hospital, Healthcare, High Reliability Organizations, Just culture, Learning Culture, Poudre Valley Health System, Sentara Health, Transparency Leave a comment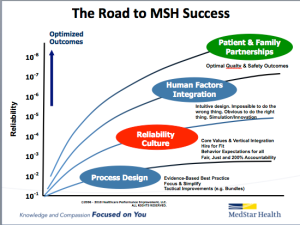 For the last twelve months, our health system has undertaken a system-wide initiative to join the ranks of healthcare organizations like Cincinnati Children’s Hospital, Poudre Valley Hospital, and Mainline Health on a journey that seeks high reliability. We have already seen the fruits of this journey, and believe that when the benefits of a High Reliability culture are combined with the expertise provided by our National Center for Human Factors in Healthcare, led by Terry Fairbanks MD, MS, along with the guidance provided by our National Patient and Family Advisory Council for Quality and Safety, exciting opportunities to improve quality and safety while reducing cost can be realized.
For the last twelve months, our health system has undertaken a system-wide initiative to join the ranks of healthcare organizations like Cincinnati Children’s Hospital, Poudre Valley Hospital, and Mainline Health on a journey that seeks high reliability. We have already seen the fruits of this journey, and believe that when the benefits of a High Reliability culture are combined with the expertise provided by our National Center for Human Factors in Healthcare, led by Terry Fairbanks MD, MS, along with the guidance provided by our National Patient and Family Advisory Council for Quality and Safety, exciting opportunities to improve quality and safety while reducing cost can be realized.
An important part of this journey includes creating a learning culture built on transparency that many in healthcare are still uncomfortable with. Overcoming these barriers requires consistent and repetitive role-modeling and messaging around core principles that help instill and reward open and honest communication in an organization. One of the ways we continue to reaffirm these important messages is through our “60 Seconds for Safety” short video series, which highlights different high reliability and safety principles. Each week, a video from the series is attached to our “Monday Good Catch of the Week” email, delivered throughout our system. The video highlights one important safety message all our associates can become more familiar with, and hopefully apply as they go about their daily work that week. Similar to starting every meeting with a safety moment, we want all of our associates to start each new week with an educational message reminding us that safety is our number one priority. The videos are available on MedStar’s YouTube Channel, under the Quality & Safety playlist. Please feel free to use any of these videos in your own Quality & Safety work — and please share ways you are getting the quality & safety message out to your front line associates.
Healthcare 2.0 Borrowing Management 2.0 Tactics
Posted: September 10, 2012 Filed under: High Reliability Organizations, Leadership, Medical Education, Transparency | Tags: Healthcare 2.0, Leadership, Management 2.0, Transparency Leave a commentOn the Harvard Business Review Blog Network last week, Jordan Cohen’s piece, “Love, Trust, and Candor: Today’s Management Priorities” outlines how love, trust and candor facilitate business operations. Having attended the Management Innovation eXchange, aka (MIX) Mashup in June of this year, Cohen reflects on how the new business leadership values have a foundation in trust and transparency. He writes:
John Mackey, founder of Whole Foods, often speaks about finding “friendship, love and community” in the workplace, Zappos CEO, Tony Hsieh, is famous for believing that we “function best when we can be ourselves” and Vineet Nayar, CEO of HCL, radically promotes “creating trust…by pushing the envelope of transparency.”
These same values — transparency, trust and open, honest communication — are being called for within healthcare as the foundation for patient-centered care. Without trust on both sides of the doctor-patient relationship, outcomes have become less than optimal–as they have in some areas of the business sector. By inviting patients into the care team to share their knowledge, as well as commit to the treatment plan prescribed as a full partner with complete knowledge of risks, benefits and alternatives has potential to elevate the entire healthcare team’s capabilities, similar to the results Cohen references.
In his article, Cohen also refers to Management 2.0, a concept described by Gary Hamel in the Wall Street Journal blogs that encourages leaders to “retool management systems and processes that govern…”
- How strategies get created
- How opportunities get identified
- How decisions get made
- How resources get allocated
- How activities get coordinated
- How power gets exercised
- How teams get built
- How tasks and talent get matched up
- How performance gets measured
- How rewards get shared
Healthcare 2.0 is in the works, but it has to address more than just the IT piece. The management piece is equally important, and based on much of what is occurring in pockets across the country, we’re already headed in that direction. Aren’t the following healthcare processes and systems also being retooled:
- Changing hospitals into high reliability organizations
- Restructuring the provider-patient relationship to include open, honest discussion and transparency
- Reorganizing business models
- Re-tooling medical education and addressing deficits
- Developing multi-disciplinary care teams
- Better management of resources
- Pay for performance…
This list suddenly looks very familiar.
Change takes time, and real leadership to navigate the fear that creates obstacles en route to success. But change is inevitable as the saying goes…and is well in motion across industries, as the new and/or evolved leaders share below.
Seth Godin speaks of “Tribes” and of leading niches versus building business models that strive to be one size fits all solution.
Eric Topol is calling for the “Creative Destruction of Medicine”
And Atul Gawande asks for “disruptive innovation” in medicine.
All collectively speak to recreating current operating models to address the changing needs of today — in business and in healthcare. Healthcare 2.0 is already well on its way…
What Leaders Are Saying About the HRO Journey and Transparency
Posted: July 14, 2012 Filed under: High Reliability Organizations, Transparency | Tags: High Reliability Organizations, Leadership, Transparency Leave a commentCincinnati Children’s Hospital has been on their high reliability journey for a number of years. As such, they have embraced transparency as one of their five defining characteristics along with: 1) Leadership 2) Institutional infrastructure, organizational alignment, and resource investment 3) Rigorous measurement and 4) Accountability.
Here’s what they had to say about transparency in the AHRQ report I shared in yesterday’s post.
In a culture that stresses continuous improvement, easy and open access to information is essential. Like other organizations that have embraced high reliability organizing, Cincinnati Children’s embraces the belief that open communication is necessary for its transformation to succeed. The following are key aspects of transparency:
- Transparency must span all levels of the organization. Holding information about organizational successes and failures at the leadership level often can be counterproductive. If you don’t make information available to all staff, they cannot fully participate in rapid-cycle improvement. Moreover, in order to motivate staff to change behaviors and give them freedom to think creatively about potential improvements, they need full access to information about what is working well and what could be working better. Once information is shared, the opportunity exists to actually address the underlying cause.
- Transparency must include recognition of successes as well as failures. Improvement can only occur if failures are identified and addressed, but building a culture of trust that encourages staff to report failures is difficult. Cincinnati Children’s has worked with one unit in particular to increase reliability and celebrate successes. When a near-miss event takes place and a staff member accurately records the event, that staff member is acknowledged for reporting the event. Because continuous improvement efforts will entail both successes and failures, communicating about both is essential for transformation to occur.
- Transparency should include patients and families. Sharing information with patients and families can actually alleviate questions and concerns that may arise during the course of care. The key is to ensure that any information shared is presented in a way that is meaningful to the families and is easily understood. Involving families in organization wide advisory councils and unit-based improvement teams is an effective way of sharing information and soliciting feedback on opportunities for improvement. In some units of systems in the HRO Learning Network, information about unit performance is posted in public locations where it can be seen by patients and their families.
- Transparency should occur through multiple media. Reporting information in multiple locations and through multiple media increases the odds that the information will be seen by a larger audience. Cincinnati Children’s takes advantage of bulletin boards, computer screen savers, its intranet, and the Internet to share information with staff, patients, and families. Although it is a challenge, the organization has made a commitment to posting information in ways that patients and their families will be able to understand and use.
Excellent insights on the power of transparency in leading change towards clinical care excellence. Great things usually happen when people are transparent about their outcomes and can learn from the data. Transparency is also about having open and honest conversations between caregiver and patients…even at the most difficult of times. We have always believed transparency starts with the first conversation between patient and caregiver. From informed consent (or preferably shared decision-making) to end-of-life discussions, understanding a patient’s preferences, values, needs and goals helps set the stage for truly transparent and un-biased conversations that produce meaningful decisions. More on transparency as it relates to open and honest communication in informed consent to follow.
High Reliability Series: The Need For Transparency
Posted: July 13, 2012 Filed under: High Reliability Organizations, Transparency | Tags: High Reliability Organizations, Transparency 1 Comment
At 0:43 in the YouTube clip above, Bob Galbraith, MD, and Executive Director, Center for Innovation at the National Board of Medical Examiners says:
“If we don’t talk about our mistakes, we’re doomed to repeat them. Over and over and over again. So we have to have transparency and admit that we’ve made a mistake in order to prevent that mistake from ever happening again. And if we don’t do that, shame upon us.”
Transparency is a core characteristic of high reliability organizations. How can an organization improve if those leading the way do not expect and set the course for a culture that embraces honest assessment of operations and open, honest communication around the good, the bad and the ugly? The first step to change is admitting there is a problem–it’s Psychology 101. If organizations fail to admit, or even see, there is a problem the journey to high reliability never gets off the ground.
AHRQ has put out an excellent set of guidelines for the HRO journey, “Becoming A High Reliability Organization: Operational Advice For Hospital Leaders”. In it, Exempla CEO Jeff Selberg says that transparency is the key to culture change, and that an “unwillingness to face and share the hard facts is an indicator of denial, and denial is not compatible with a safe environment.”
Transparency sets the foundation and tone within an organization for every aspect of daily operations. Reporting of outcomes, reporting of near misses and unsafe conditions, management of medical error, interprofessional communication, patient-centered care–all of these operating procedures are limited, or reach new heights, in direct relationship to the level of transparency within an organization.
The challenge to create a truly transparent culture is a “must have” for any HRO–and as Paul Levy wrote in yesterday’s post, An Interest In Remaining Alive, a challange to hospital systems around the world. A healthcare culture that remains opaque will continue to harm patients–it’s occurring far too frequently in every corner of the globe. In the end, this is what we all swore to do when we received our MD–to first do no harm. Honing the characteristics of a HRO, starting with transparency, will help move healthcare to a state of being that will make patients feel they are as safe as they are on airplane when they enter a hospital.
More on transparency tomorrow…
Resident Physician & Health Science Student Summer Camp in Telluride, CO: What’s It All About?
Posted: June 17, 2012 Filed under: Medical Education, Patient Safety, Transparency | Tags: Culture change, Medical Education, Patient Safety, Resident Physicians, Transparency Leave a commentMany have asked about the Telluride Patient Safety Educational Roundtable and Resident Physician/Health Science Student Summer Camps mentioned in previous posts. In short summary, interprofessional leaders in patient safety, patient advocacy, and health science education have come together in Telluride, CO for the last eight years to address educational challenges around patient safety. The original Telluride Vision–still true today–was to create an annual retreat where stakeholders in patient safety, patient advocacy and health science education can come together in a relaxed and informal setting to discuss, develop and refine curricula that support a culture of patient safety, transparency and optimal outcomes in health care.
The theme the last few years has focused on The Power of Change Agents: Teaching Caregivers Open, Honest and Professional Communication Skills to Overcome the Multiple Barriers to Patient Safety and Transparency. Through the generous support of AHRQ, COPIC, the Committee of Interns and Residents, and in particular The Doctors Company Foundation (TDCF) and MedStar Health, we have been able to add Patient Safety Summer Camps for health science students and resident physicians. This year, funding from these organizations is allowing us to sponsor 70 students and residents each to attend one of three week-long Summer Camps, where our focus truly is educating the young.
For more information on the recent Resident Patient Safety Summer Camp activities, I encourage you to visit Paul Levy’s blog Not Running A Hospital. Paul spent last week at our resident physician summer camp, and posted a number of stories about his experience with the residents while in Telluride.
Student and faculty daily reflections and comments can also be found on the Transparent Health blog.
Learning objectives for 2012 Summer Camps will enable the residents and students to:
1. Describe at least three reasons why open, honest and professional communication between caregivers, patients and family members is critical to patient safety, transparency and reducing harm in healthcare.
2. Utilize tools and strategies to lead change specific to improving communication and reducing patient harm.
3. Implement, lead and successfully complete a Safety/QI project at their institution over the next twelve months.
The passion and excitement exhibited by these young caregivers is contagious. Over the course of the week, they engage in both structured and informal discussions, addressing a wide range of issues related to transparency and patient safety. When the week is finished, they reflect and share their thoughts with all attendees.
Every one of the student reflections is powerful, providing insight into the front lines of medical education. I wanted to share one reflection from the residents’ week that captures the essence of the Telluride Summer Camps:
“If I had spent the last four days locked in a library researching the patient safety literature non-stop, I would not have walked away with as much knowledge, enthusiasm, and support as I acquired participating in the Transforming Mindsets: Patient Safety Summer School for Resident Physicians in Telluride, Colorado. The collective efforts, shared experience, and mutual support of everyone involved made for a special atmosphere (in the already special atmosphere of nine thousand feet) that allowed each of us to rise above our prior potentials. Within an hour of resuming clinical duties today, I was already championing our collective cause, walking a fourth year medical student through an incident report about a delayed dose of nevirapine in a newborn; her initial grimace at the optional “name of reporter” question eventually morphing into an enthusiastic smile as she entered her name following our discussion about the benefits of reporting and transparency. I couldn’t be more excited right now to motivate these types of small shifts towards a safety mindset while also pursuing large-scale systems shifts that ensure safety as well. Thank you to the faculty and especially to the other residents!”
For information on next year’s Telluride Patient Safety Roundtable and Summer Camps, email: david.b.mayer@MedStar.net and have a look at the following short film from last year’s summer camp which captures student and faculty comments about their experience.
We Are All Students
Posted: June 12, 2012 Filed under: Healthcare Quality, High Reliability Organizations, Just Culture, Leadership, Medical Education, Medical Error, Patient Advocacy, Patient Safety, Transparency | Tags: Honest Communication, Medical Education, Medical Error, Patient Safety, Transparency Leave a comment The educational value of narrative and reflective learning is well documented in the literature. These educational powers are especially true in healthcare when teaching health science students and resident physicians risk reduction strategies in the provision of safe, high quality patient care. Wall of Silence, written by Rosemary Gibson, demonstrates this educational power extremely well. The book shares numerous cases where medical error caused significant, many times fatal, patient harm. Unlike traditional medical case reviews discussed in M&M’s or written for journal publication, the book takes a different approach to these cases and shares through interviews what patients and family members expected from caregivers after good intentioned care caused harm. The take-away from these patient and family interviews highlight five areas of need:
The educational value of narrative and reflective learning is well documented in the literature. These educational powers are especially true in healthcare when teaching health science students and resident physicians risk reduction strategies in the provision of safe, high quality patient care. Wall of Silence, written by Rosemary Gibson, demonstrates this educational power extremely well. The book shares numerous cases where medical error caused significant, many times fatal, patient harm. Unlike traditional medical case reviews discussed in M&M’s or written for journal publication, the book takes a different approach to these cases and shares through interviews what patients and family members expected from caregivers after good intentioned care caused harm. The take-away from these patient and family interviews highlight five areas of need:
1. The truth
2. Accountability
3. An apology when appropriate
4. Remedy
5. Commitment (and action) to change the system to protect others from similar harm.
Patients and family members are great teachers and educators. Lessons learned from these stories through the patient’s voice are powerful teaching tools that survive the educational decay commonly seen with traditional teaching methodologies. While these are all tragic stories, there is much to be learned when we as caregivers are willing to hear what our patients tell us and engage in truthful and transparent discussion. As Rosemary told me many years ago, the best teachers find ways to connect the brain to the heart and leave a lasting educational imprint on their students.
