The Happiness Advantage Applied to Healthcare
Posted: May 26, 2015 Filed under: Healthcare Innovation, Leadership, Patient Centered Care, Patient Experience | Tags: happiness, Healthcare, Healthcare Leadership, Shawn Achor Leave a commentWhat if this was the norm in healthcare? At the frontlines between and among colleagues, and maybe most importantly, the feeling conveyed to patients when they walked onsite? Could it restore joy and meaning? Could it make care safer? Isn’t it worth a try?
Something to put a smile on your face as we kick off the new week and season!
Patients and Care Teams: Working Together at MedStar Health
Posted: April 20, 2015 Filed under: High Reliability Organizations, Just Culture, Leadership, Patient Advocacy, Patient Centered Care, Patient Safety | Tags: Compassion, Healthcare, High Reliability Organizations, MedStar Health, Patient Partnerships, Please See Me, YouTube Leave a commentAs healthcare providers, we are given a privilege to care for others, and must always remember that we treat complex individuals, making choices that affect their lives, families and personal well-being. At the same time, our patients must recognize that care providers are people too– always trying to do the best they can while juggling numerous responsibilities on a daily basis and working in a system that still has too many flaws. The clinician-patient relationship is most effective when both sides meet in the middle–a “safe space” where each is able to truly see one another and achieve the mutual understanding needed to succeed as a care team.
High Reliability science is one area we are looking to for answers to systems failures in healthcare. High reliability organizations stress the importance of “Stopping the Line” when a worker senses something doesn’t feel right. The concept has been shown to help reduce harm in many high risk environments. What if something similar existed for communication concerns in the healthcare environment?
The following short video, entitled Please See Me, created by patients and caregivers for patients and caregivers, offers a possible solution. Can “Please See Me” become that safe space, where patients and family members can stop the line and share those words if they feel their needs are not being heard or addressed? At the same time, can caregivers use the same phrase when they feel they are not being understood by patients and family members?
Many of us believe the phrase “Please See Me” can be the start of something special, creating that safe space and providing a phrase that helps improve communication and understanding in every healthcare environment leading to better outcomes.
Patients and Care Teams
Working as Partners
In the Spirit of Healing and Compassion
Role Models, Dedication and Driving Your Own Destiny
Posted: April 17, 2015 Filed under: Leadership, Medical Education, Nursing Education | Tags: Graduate Medical Education, Healthcare, Leadership, Medical Education, Role Models, Rory McIlroy, Tiger Woods Leave a commentWhether or not Tiger Woods is deserving of being called a role model, the body of work he has accumulated is worthy of admiration, especially by younger players like Rory McIlroy. What caught my attention about yet another inspiring Nike commercial, wasn’t so much the role model himself, but the reminder that others are watching and learning from the actions of those put into a leadership position–regardless of how deserving.
In healthcare, as in sport, skills and technical acumen are only part of the equation, though often they can take many onto a stage and into the spotlight exposing behavior and character far less developed. Like McIlroy, those with talent coming up the ranks in sport can often drive their own destiny with dedication and committment. Athletes can stay a safer distance from those who have gone before them than young learners and junior healthcare professionals. But these young professionals too can drive their own destiny, and shape a new set of expectations for what success looks like in healthcare. Here’s a shout out to our Telluride Alum on this Friday!
*In the event the video is pulled, you can find it on YouTube — Nike Golf, Ripple
Healthcare Transparency As A Blockbuster Drug
Posted: February 2, 2015 Filed under: Just Culture, Leadership, Patient Safety, Transparency | Tags: Healthcare, Leadership, Lucian Leape Institute, Transparency Leave a comment“If transparency were a medication, it would be a blockbuster, with billions of dollars in sales and accolades the world over. While it is crucial to be mindful of the obstacles to transparency and the tensions—and the fact that many stakeholders benefit from our current largely nontransparent system—our review convinces us that a health care system that embraces transparency across the four domains will be one that produces safer care, better outcomes, and more trust among all of the involved parties. Notwithstanding the potential rewards, making this happen will depend on powerful, courageous leadership and an underlying culture of safety.”
 The previous paragraph comes from the fifth and final National Patient Safety Foundation’s Lucian Leape Institute (LLI) White Paper entitled, “Shining a Light: Safer Health Care through Transparency”. Each of the five white papers address key issues that healthcare stakeholders will need to successfully manage if healthcare is to achieve zero preventable harm. I was honored to be part of the panel that helped create this paper and the 39 recommendations for greater transparency throughout healthcare.
The previous paragraph comes from the fifth and final National Patient Safety Foundation’s Lucian Leape Institute (LLI) White Paper entitled, “Shining a Light: Safer Health Care through Transparency”. Each of the five white papers address key issues that healthcare stakeholders will need to successfully manage if healthcare is to achieve zero preventable harm. I was honored to be part of the panel that helped create this paper and the 39 recommendations for greater transparency throughout healthcare.
Defining transparency as “the free, uninhibited flow of information that is open to the scrutiny of others”, the paper provides recommendations in four different domains of transparency:
- Transparency between clinicians and patients (illustrated by disclosure after medical errors)
- Transparency among clinicians themselves (illustrated by peer review and other mechanisms to share information within health care delivery organizations)
- Transparency of health care organizations with one another (illustrated by regional or national collaboratives)
- Transparency of both clinicians and organizations with the public (illustrated by public reporting of quality and safety data)
I encourage everyone to visit the LLI website and download the White Paper (click here for a copy). Increased transparency is critical to any Patient Safety mission. Greater transparency throughout the system is not only ethically correct, but will lead to improved outcomes, fewer errors, more satisfied patients, and lower costs.
Leading From the Heart
Posted: December 31, 2014 Filed under: Leadership, Medical Education, Patient Safety, Transparency | Tags: David Mayer MD, Healthcare, Leadership 2 CommentsLeadership is not so much about technique and methods as it is about opening the heart…about inspiration–of oneself and of others. Great leadership is about human experiences, not processes…it is not a formula or a program, it is a human activity that comes from the heart and considers the hearts of others. It is an attitude, not a routine.
Lance Secretan
Secretan’s teachings are based on the core principle of connecting the soul with what we consider as “work”– the two becoming intertwined in a way that redefines our “work-life” balance, making both truly fulfilling. It combines our inner passion to make a difference in someone’s life with our reason to get up each morning and go to “work”.
Each day in healthcare we are given the opportunity to make the world a better place—for our patients, our colleagues and our communities. As healthcare providers, we entered into our profession to care for others–to keep our patients safe at all costs while under our care. Think of the healing power that could occur not only in our healthcare workforce, but also in our patients, if leaders created care environments that were truly places that nurtured the soul.
Rosemary Gibson said it best when she paraphrased Gandhi, reminding us: “A patient is the most important visitor on our premises. They are not dependent on us – we are dependent on them. They are not an interruption in our work – they are the purpose of it. We are not doing our patients a favor by serving them, they are doing us a favor by allowing us to serve them.”
Can healthcare leaders create a work environment that reflects and honors the creative spaces of the soul and brings passion back into our daily work? Can healthcare leaders inspire caregivers to connect with their own inner values in helping health systems achieve the highest quality, safest care possible for both patients and caregivers?
As we move into the New Year, I am hopeful we can all “lead from the heart” in ways that inspire ourselves and others to achieve the highest quality, safest care possible for our patients and our caregivers.
Wishing everyone a healthy and happy new year.
Virtual Stocking Stuffer for Storytellers
Posted: December 19, 2014 Filed under: Leadership, Medical Error, Storytelling | Tags: Healthcare, Leadership, Medical Error, Storytelling Leave a comment After a brief hiatus for the #IHI26Forum, and in preparation for launch of Using Stories to Influence Change in Healthcare as an Amazon eBook, we are back online! With all the repeat hits to our ETY storytelling posts, it seemed of value to put them in a collection along with some of the ‘how and why’ storytelling has become of even greater value in healthcare. Here is the link if interested in having all of the storytelling posts in one place along with new commentary. From the description:
After a brief hiatus for the #IHI26Forum, and in preparation for launch of Using Stories to Influence Change in Healthcare as an Amazon eBook, we are back online! With all the repeat hits to our ETY storytelling posts, it seemed of value to put them in a collection along with some of the ‘how and why’ storytelling has become of even greater value in healthcare. Here is the link if interested in having all of the storytelling posts in one place along with new commentary. From the description:
…as long as there are patients who fall victim to preventable harm in healthcare, there are healthcare professionals who also have a story rich in learning material from the other side of the bedrail. Both sides of the patient harm story will need to be embraced by healthcare leadership in order to achieve the delivery of reliable, high-quality, safe care everyone desires. Because the numbers harmed by healthcare have at the very best plateaued, an urgent need to pick up the pace for change remains. Sharing the stories of patients and healthcare professionals on a larger and more strategic scale throughout the industry will allow others to learn vicariously from mistakes as well as successes, building upon the positive momentum found when utilizing storytelling as a medium for change. Once again, our stories can provide the guiding light leading us into a new world for healthcare—where the patient voice is welcomed, and healthcare professionals are allowed to speak their truth.
And finally, our healthcare stories also serve many masters. When patients share their story of illness, they heal. When families tell stories of loss, they grieve. When healthcare professionals relate stories of guilt or near misses, they unburden their souls and can fix what is broken in health systems, enabling them to once again care for others as intended. Freedom to tell our story has always been a way to health and happiness. Using Stories to Influence Change in Healthcare is a jumping off place for those interested in learning more about how stories are being used in healthcare, and why they hold the power over us that they do. Tips from expert storytellers on how to craft good stories, as well as a glimpse into the science of story round out this introductory collection on using stories in healthcare…
Residents as Sentinels and Change Agents for Safer Care
Posted: April 21, 2014 Filed under: Leadership, Medical Education, Patient Safety | Tags: Carole Hemmelgarn, CIRSEIU, David Leach, David Mayer, Graduate Medical Education, Healthcare, Healthcare Quality, Resident Physicians, Rosemary Gibson 1 CommentThis coming Saturday, April 26th, the Committee of Interns and Residents (CIR) will be hosting its next QIIQ Conference titled, “How to be a Lead Agent of Change: From Bedside to Transformative Care“, in NYC. Rosemary Gibson, Carole Hemmelgarn, Shelly Dierking and I have the honor of joining leaders from CIR to help facilitate the all-day interactive session. While many faculty will be attending, the major focus of this educational meeting will be on the residents, both from CIR Hospitals as well as other GME programs, and aligns with the “Educating the Young” mission.
Residents can be change agents for safer, higher quality care. There are now numerous examples across the country of this fact–residents leading important quality and safety initiatives that have reduced risk and raised the quality of care provided–and they have done this work despite internal challenges and long work weeks. Those that have followed our ETY blog for the past two years will remember my post on the work of David Leach, the former CEO for the ACGME (see The Canary in the Coal Mine…). In one of his publications, Dr. Leach shared the most important role of graduate resident physicians was to act as the “moral agent” for their patients. Residents must be the gatekeepers for safe, high quality care–a sentinel on watch for the many unsafe conditions they might encounter while trying to provide optimal patient care, prepared to alert faculty and leadership to these unsafe conditions, and then work with their institutions to find solutions to remove risk from the patient experience. The analogy Dr. Leach used was the canary in the coal mine, taking on the role of guardian and protecting others from harm before it was too late. I loved this “moral agent” concept. It is so simple, yet so important in the quest for safer, higher quality, patient care. In academic medical centers, resident physicians spend more time in the hospital, have more direct contact with patients, and see many more unsafe conditions during days, evenings and weekends than most other caregivers, except possibly nurses. And they do it many times with little, if any, direct supervision. Resident physicians can be those sentinels and serve as excellent change agents for safer care.
We need more conferences like CIR’s QIIQ focused on our next generation of caregivers. Please help spread the word about the conference. Below is some additional background information with the links to register. The third link is the conference brochure which has additional details. We appreciate the support and as always, thank you!!
Background Info:
The one-day conference on How to be a Lead Agent of Change will be held Saturday, April 26th in New York City. Given the importance of the patient experience and the desire for more patient-centered care, the Committee of Interns and Residents conference is meant to empower medical residents to develop and execute high-value care projects in their hospitals and health systems, and better equip them with the competencies they need to work in a rapidly changing delivery system.To register for this conference, please click here. There will also be a webcast, and people can sign up for that here. The agenda and conference brochure can be found here (this includes logistics on location and timing, as well as goals for the day and additional contact information). Please feel free to share this information, as well as the links to register, with your organization and networks.
*CIR has also been tweeting about the conference with the #QIIQ hashtag. Here is a sample tweet you are more than welcome to share with your followers: What’s your #QIIQ? Join @cirseiu & @EinsteinMed in NYC on 4/26 for the next #QIIQ conference. Register now! bit.ly/qiiq426
Teamwork and Thinking Differently: Can Healthcare Leaders Do This?
Posted: April 17, 2014 Filed under: Healthcare Innovation, Just Culture, Leadership | Tags: Healthcare, Leadership, Music, Teamwork, YouTube 1 CommentIf you can make it to “When the Shark Bites…” you’ll have already seen what teamwork looks like in this talented quartet. A piano has just 88 keys, yet new music is created every day. How can we take what we have to work with in healthcare and see what has yet to be discovered or apply what has yet to be tried — especially when it comes to teamwork.
Please share creative examples of how your health system is applying teamwork!
Telluride Faculty Member Dr. Kim Oates: On Kindness in Healthcare
Posted: April 7, 2014 Filed under: Just Culture, Leadership, Patient Safety | Tags: Graduate Medical Education, Healthcare, Kim Oates MD, Kindness, Leadership, Medical Education, Patient Safety 2 Comments Kim Oates MD has been a regular faculty member at the Telluride Patient Safety Educational Roundtable and Summer Camps, which is no easy accomplishment given he travels to this remote Rocky Mountain town all the way from Australia. Kim, who is a pediatrician by training, is a medical educator to the core, and is now Emeritus Professor, Director Undergraduate Quality & Safety Education, Clinical Excellence Commission in New South Wales. The following is an excerpt from a piece he wrote on kindness in healthcare for the Royal Australasian College of Physicians, recently reprinted in the Medical Journal of Australia. Please feel free to share with colleagues. The entire abridged piece in MJA can found by clicking here.
Kim Oates MD has been a regular faculty member at the Telluride Patient Safety Educational Roundtable and Summer Camps, which is no easy accomplishment given he travels to this remote Rocky Mountain town all the way from Australia. Kim, who is a pediatrician by training, is a medical educator to the core, and is now Emeritus Professor, Director Undergraduate Quality & Safety Education, Clinical Excellence Commission in New South Wales. The following is an excerpt from a piece he wrote on kindness in healthcare for the Royal Australasian College of Physicians, recently reprinted in the Medical Journal of Australia. Please feel free to share with colleagues. The entire abridged piece in MJA can found by clicking here.
Way back in my intern days, it was unusual for consultants to talk with their “public” patients…The hard stuff was often left to us — the interns, young people with minimal life experience, an overwhelming workload and no training in the gentle art of communication.
At my teaching hospital a time was set aside once each week when family members could come to the hospital foyer, page the intern and ask questions about their loved one’s condition. In my third month after graduation I assisted at a laparotomy on a fit, active 54-year-old man who presented with a hard lump at his umbilicus. The laparotomy showed widespread cancer with multiple metastases. The surgeon closed the wound. There was nothing to be done…It was my job to tell his unsuspecting wife when she came to the foyer to ask about her husband’s operation. I told her the truth as kindly as I could. Her eyes welled up with tears. So did mine.
Afterwards, I felt embarrassed about my show of emotion. Why couldn’t I be “more professional” like my consultants? I wondered if I was really suited to do medicine. Later, I realised that it may have helped her. She may have seen that even though the news was bad, I cared…In subsequent years, as a consultant, my eyes would sometimes moisten when I had to tell a parent that their child would not survive. And sometimes it happened when I had the pleasure of giving unexpected, but joyful news.
Was this behaviour “unprofessional”? Or is there is room for families, junior doctors and medical students to realise that we, the more senior doctors, do care? To realise that there is more to it than striding the narrow catwalk between aloofness and over-familiarity, that there is a place to show humanity and that it is not unprofessional to let people know we care…
…Of course, there are some professional boundaries which we must always respect…these well accepted boundaries are different from really caring about our patients and doing something about it…We don’t have to take off our compassion, or our ability to show it, when we drape a stethoscope around our neck. The need for doctors to be professional is not synonymous with being emotionless. There is more to this than just being nice to people. It is about being kind. It also has implications for the quality of patient care…
Powerful recommendations — listen to patients; model transparency; model trust; keep on learning.
Continuing a Journey That Seeks High Reliability
Posted: February 24, 2014 Filed under: High Reliability Organizations, Just Culture, Leadership, Uncategorized | Tags: Cincinnati Children's Hospital, Healthcare, High Reliability Organizations, Just culture, Learning Culture, Poudre Valley Health System, Sentara Health, Transparency Leave a comment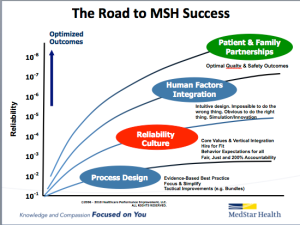 For the last twelve months, our health system has undertaken a system-wide initiative to join the ranks of healthcare organizations like Cincinnati Children’s Hospital, Poudre Valley Hospital, and Mainline Health on a journey that seeks high reliability. We have already seen the fruits of this journey, and believe that when the benefits of a High Reliability culture are combined with the expertise provided by our National Center for Human Factors in Healthcare, led by Terry Fairbanks MD, MS, along with the guidance provided by our National Patient and Family Advisory Council for Quality and Safety, exciting opportunities to improve quality and safety while reducing cost can be realized.
For the last twelve months, our health system has undertaken a system-wide initiative to join the ranks of healthcare organizations like Cincinnati Children’s Hospital, Poudre Valley Hospital, and Mainline Health on a journey that seeks high reliability. We have already seen the fruits of this journey, and believe that when the benefits of a High Reliability culture are combined with the expertise provided by our National Center for Human Factors in Healthcare, led by Terry Fairbanks MD, MS, along with the guidance provided by our National Patient and Family Advisory Council for Quality and Safety, exciting opportunities to improve quality and safety while reducing cost can be realized.
An important part of this journey includes creating a learning culture built on transparency that many in healthcare are still uncomfortable with. Overcoming these barriers requires consistent and repetitive role-modeling and messaging around core principles that help instill and reward open and honest communication in an organization. One of the ways we continue to reaffirm these important messages is through our “60 Seconds for Safety” short video series, which highlights different high reliability and safety principles. Each week, a video from the series is attached to our “Monday Good Catch of the Week” email, delivered throughout our system. The video highlights one important safety message all our associates can become more familiar with, and hopefully apply as they go about their daily work that week. Similar to starting every meeting with a safety moment, we want all of our associates to start each new week with an educational message reminding us that safety is our number one priority. The videos are available on MedStar’s YouTube Channel, under the Quality & Safety playlist. Please feel free to use any of these videos in your own Quality & Safety work — and please share ways you are getting the quality & safety message out to your front line associates.
